Virtual consultations have become an integral part of healthcare delivery. However, their continued success depends on measuring their performance effectively. My research on virtual consultation adoption in the NHS highlights key factors influencing their sustained use, aligning with existing literature on digital health adoption.
A clear framework can help healthcare leaders, clinicians, and policymakers evaluate how well virtual consultations are working.
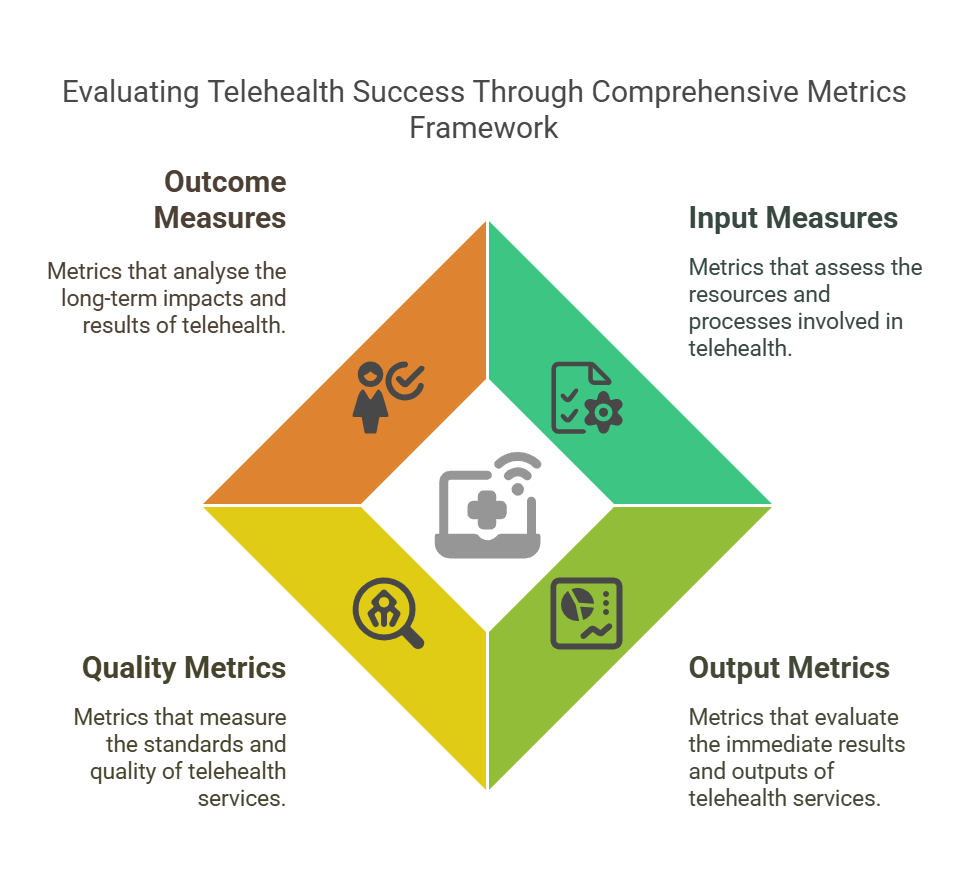
1. Input Measures (Easy to track, but don’t show full impact)
- Number of clinicians trained: Training clinicians on virtual consultation workflows and digital communication improves adoption and satisfaction.
- Number of patients checked for technology access: Ensuring patients have access to suitable devices and internet connectivity reduces technical failures and missed appointments
- Percentage of workflows defined: Clear steps for handling virtual consultations make sure they fit smoothly into normal care routines.
- Number of devices deployed: Simply giving out equipment isn’t enough; it needs to be easy to use and properly connected to appropriate systems.
2. Output Metrics (Show usage and reach)
- Total number of virtual consultations: Tracking how many virtual consultations happen in different areas (e.g., GP visits, mental health) helps identify service needs.
- Percentage of VCs completed vs. rescheduled or cancelled: helps assess whether virtual consultations are a reliable option compared to face-to-face care.
- Number of billable virtual consultations: important for financial sustainability, depending on the funding models.
- Travel miles saved: Reducing travel for patients and clinicians improves efficiency and supports NHS sustainability goals.
3. Quality Metrics (Harder to track but very useful)
- Clinician satisfaction: If clinicians find virtual consultations effective and time-saving, they are more likely to keep using them.
- Staff satisfaction: Admin teams play a crucial role in virtual consultation success. Ensuring smooth scheduling and technical support reduces stress and improves adoption.
- Patient satisfaction: While many patients like the convenience of virtual consultations, their experience depends on good communication, reliable technology, and effective care.
- Technical performance: Common issues include poor video/audio quality and system downtime, which can undermine confidence in virtual consultations.
4. Outcome Measures (Show real impact on care and service delivery)
- Missed appointment rates (DNA – Did Not Attend): Comparing virtual consultation and in-person DNA-show rates helps see if virtual consultations improve attendance.
- Conversion of cancellations to virtual consultations: When patients cancel in-person visits, offering a virtual consultation alternative can improve continuity of care.
- Care plan engagement: Virtual consultations can help patients, especially those with long-term conditions, stay engaged with their care plans.
Tracking these measures helps healthcare providers improve their virtual consultation services, making them accessible, effective, and long-lasting. My research shows that when training, ease of use, and good clinical integration are in place, clinicians are more likely to continue using virtual consultations, benefiting both staff and patients.

