Telehealth isn’t just a digital substitute for in-person appointments. It’s a complex ecosystem that requires the input and coordination of nearly every team member across a healthcare organisation. In the world of community healthcare, where my research is focused, this rings especially true. Delivering virtual consultations at scale relies on more than just clinicians and patients logging onto a video platform. Behind every telehealth appointment is a web of workflows supported by appointment schedulers, administrators, nurses, IT specialists, and senior leaders.
Training isn’t just a tick-box exercise for clinicians. Everyone has a role in shaping the telehealth experience — and to make it work smoothly, everyone needs to understand how their piece fits into the wider puzzle.
Why does telehealth training matter to everyone?
Think of a new clinician or administrator joining your organisation. What would they need to know to be fully ready to deliver or support telehealth services confidently? It’s rarely as simple as logging into a video platform. There’s a rich tapestry of knowledge and skills behind effective virtual care delivery.
Through my research into virtual consultations in community health, I’ve found that while much attention is given to clinical effectiveness and technology, training often gets sidelined. Yet, gaps in training can be the hidden reason behind operational friction and poor adoption rates. If everyone isn’t trained, the service suffers — from scheduling issues to sub-par patient experiences.
What does effective telehealth training cover?
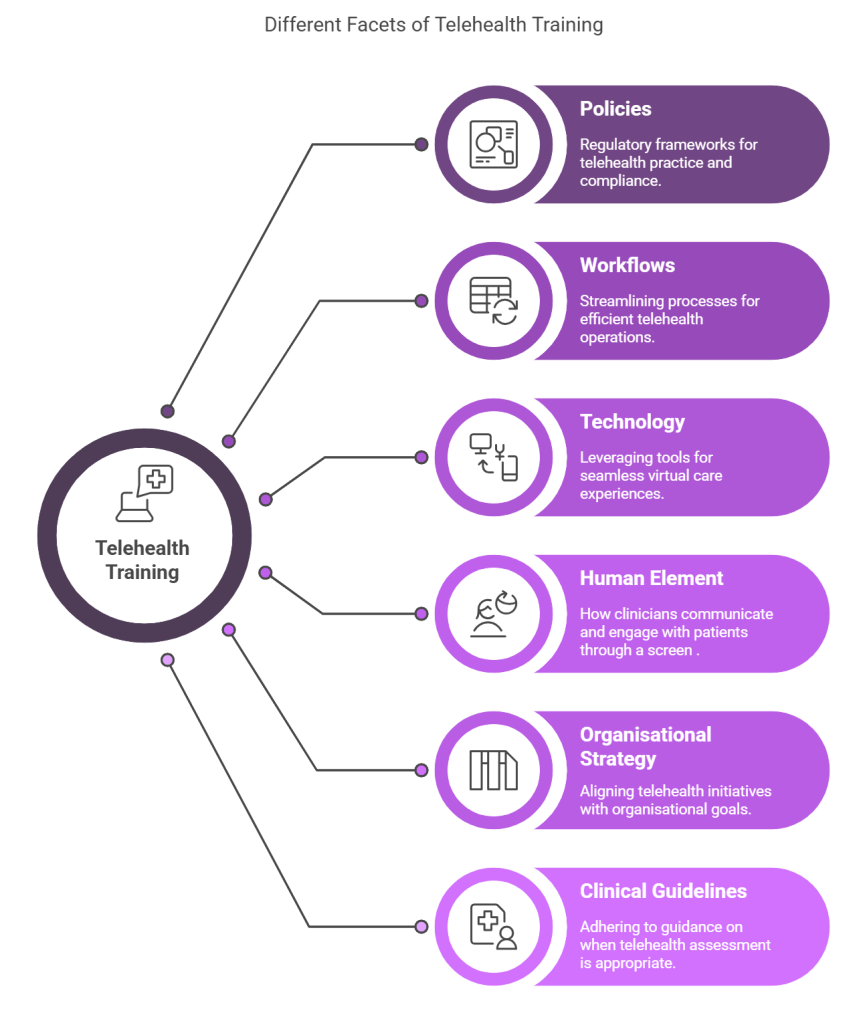
Telehealth is more than technology. It encompasses clinical, operational, and technical layers that all need attention. Let’s break it down.
First, there are the policies. Staff need to understand the regulatory frameworks, data protection requirements, and compliance rules that underpin virtual care. In the UK, this might include adhering to NHS Digital Clinical Safety standards, CQC requirements, Information Governance compliance and local Trust policies.
Then, there are workflows. Scheduling virtual consultations, managing patient communications, and triaging cases all have nuances in a telehealth model. The patient journey looks different when conducted remotely — and so do internal processes.
Technology is the next layer. Whether it’s Microsoft Teams, Attend Anywhere, or bespoke telehealth platforms, the tools need to be second nature to staff. This includes not just clinicians but also patient service teams and IT support, who often help troubleshoot issues in real-time.
There’s also the human element — often overlooked. Virtual consultations aren’t just about technical competence; they require excellent ‘webside manners.’ How clinicians communicate and engage with patients through a screen affects patient trust, satisfaction, and even clinical outcomes. My interviews with clinicians highlighted how some felt less confident interpreting non-verbal cues remotely or navigating sensitive conversations online. This is where role-play and peer feedback in training sessions can make a real difference.
On top of that, clinical teams need guidance on when telehealth is appropriate and when an in-person assessment is essential. Clinical guidelines tailored to each specialty help clinicians make safe, pragmatic decisions.
Finally, training must tie into a broader organisational strategy. If teams understand the ‘why’ behind telehealth — whether it’s reducing carbon emissions by cutting travel, improving access for patients in remote areas, or managing clinic capacity more effectively — they’re more likely to buy in and engage with the service.
A layered approach to telehealth education
In practice, training needs to be multi-layered. Different roles will require different levels of depth. For example, while a nurse or GP might need to master both the technology and clinical decision-making aspects, a patient service representative may focus more on scheduling processes and patient communications.
From my research, I’ve seen organisations that successfully scale telehealth take a phased approach. They deliver foundational awareness sessions for all staff, then follow up with targeted, role-specific training. For clinicians, this might mean peer-led workshops on virtual examination techniques. For administrative teams, it could be a walkthrough of updated booking workflows and patient onboarding processes.
One of the teams I interviewed as part of my research adopted this staggered approach. They saw a sharp reduction in virtual appointment DNAs (Did Not Attend). This was achieved after providing additional training to its admin staff on guiding patients through the telehealth set-up process.
Don’t forget the patient
While we often focus on the workforce, patients also need guidance to navigate virtual care confidently. Simple ‘tech checks’ — a short orientation call before the appointment — can dramatically improve a patient’s experience. This was evident in my research, where clinicians noted how technical hiccups often consumed the first few minutes of a video consultation, eating into valuable clinical time. Offering patients a quick, friendly tutorial beforehand can ease anxiety and ensure smoother appointments.
Building trust and breaking resistance
One finding from my research stood out: clinicians who felt undertrained in telehealth often expressed hesitancy or frustration about its use. Many linked this to uncertainty around how to conduct a remote examination effectively or manage difficult conversations through a screen.
For organisations facing pushback on virtual consultations, investing in training that focuses on these softer skills can shift attitudes. Role-modelling by senior clinicians and providing safe spaces for peer learning helps build trust in the process.
Telehealth success starts with your people
The technology may be the enabler, but it’s people who deliver the care. Every team member contributes to the patient journey, from first contact to follow-up. Investing in holistic, organisation-wide telehealth training creates a stronger foundation for delivering safe, effective, and patient-centred virtual care.
And as telehealth continues to evolve — becoming a permanent part of NHS delivery models — building these capabilities across the whole healthcare team is no longer optional. It’s essential.

