Community nurses are the backbone of home-based healthcare, ensuring patients receive essential care outside hospital settings. But their work is often burdened by inefficiencies, administrative overload, and logistical challenges. Stacey, a dedicated community nurse, experiences these struggles daily.
Let’s follow her through a typical day—first, in a traditional, paper-based system, then with digital health innovations transforming her workflow.
A Day Without Digital Health: The Paper-Based Struggle
Stacey leaves home early, heading straight to her community health office. There, she meets her colleagues and collects the day’s patient schedule—printed and arranged manually by a scheduler. She spreads out a paper map and estimates her route, factoring in potential delays. It’s a rough guess at best, with no real-time data to inform her journey.
Before setting off, she gathers the necessary medical supplies—wound dressings, blood pressure cuffs, and other essentials. She double-checks her paper notes, ensuring she has everything she might need. Once on the road, unpredictable factors come into play: traffic congestion, parking issues, and unexpected patient emergencies.
At each patient’s home, Stacey greets them warmly, conducts her assessments, and documents everything in a notebook. She makes detailed notes on vital signs, medication adherence, wound healing progress, and any concerns raised. She reassures the patient and moves to the next visit, but there’s no way to instantly update records or communicate changes with colleagues. If an urgent update is needed, she must call the office, hoping someone picks up.
By midday, she’s running behind schedule. A patient visit took longer than expected, and a last-minute request for an urgent assessment threw off her estimated timings. A delayed bus worsens the situation. She mentally adjusts her schedule, wondering if she’ll have to reschedule a later visit.
At the end of the day, Stacey returns to the office, exhausted. She logs onto her desktop and painstakingly transcribes her handwritten notes into the Electronic Patient Record (EPR) system. The process is slow and repetitive, but essential for record-keeping. By the time she signs off, it’s well past her scheduled finishing time.
This is the reality for many community nurses—time spent on administrative tasks, inefficiencies in scheduling, and potential risks to patient care due to delays in updating records.
A Day Transformed: The Power of Digital Health
Now, let’s reimagine Stacey’s day with digital health tools seamlessly integrated into her workflow.
Before she even leaves home, Stacey checks an app on her phone that has automatically scheduled her visits for the day. The system, powered by artificial intelligence, has optimised her route based on real-time traffic data and estimated visit durations. She already knows which patients she’ll be seeing, their medical history, and any specific equipment she needs to pick up.
Her first patient requires a wound check-up. As she arrives, she uses a mobile EPR system on her tablet to review their latest notes. No need to flip through pages or transcribe details later—she inputs observations directly, saving time and reducing errors. The app also flags a necessary prescription renewal, which she processes digitally in seconds.
Midway through her rounds, Stacey is notified of a patient who needs urgent attention. Instead of rearranging her entire schedule, she conducts a quick virtual check-in via secure video call. The patient, an elderly man with chronic obstructive pulmonary disease (COPD), is wearing a remote monitoring device that transmits his oxygen levels in real time. The readings suggest no immediate risk, so Stacey advises minor adjustments and schedules an in-person visit for later in the week. Without digital health, this would have required a rushed, unplanned visit, disrupting other patient care.
With each visit, Stacey seamlessly updates patient records through voice-to-text dictation on her mobile EPR system. She no longer has to return to the office for end-of-day documentation—allowing her to spend more time with patients and finish work on time.
How Digital Health Improves Patient Care and Clinician Wellbeing
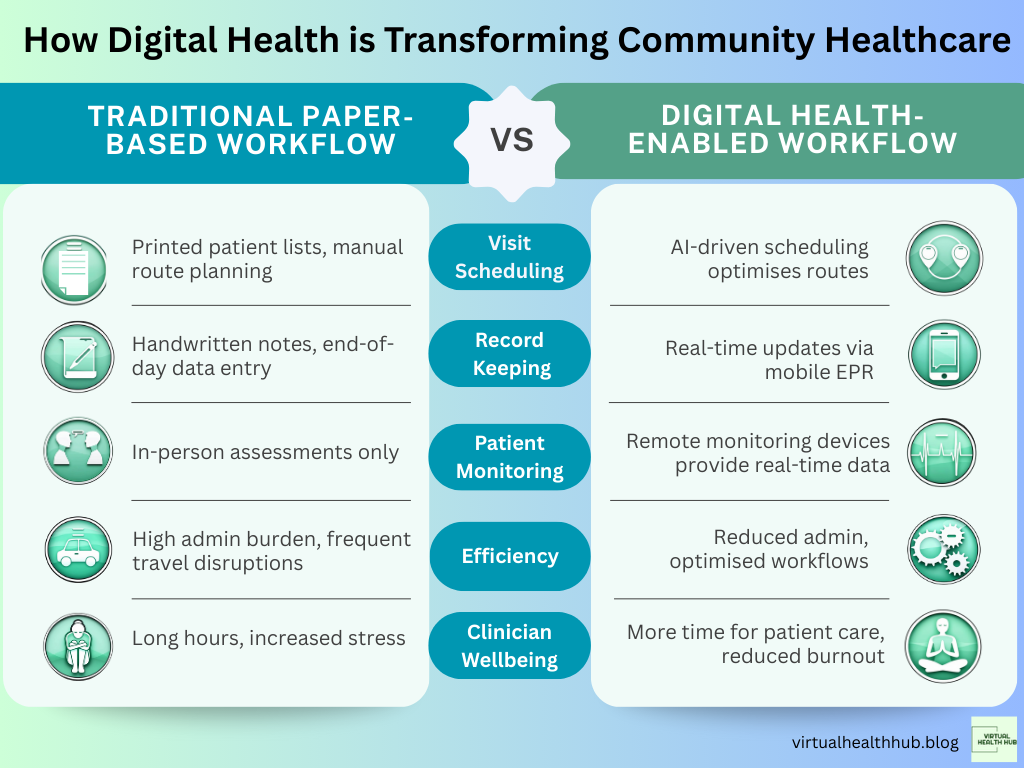
The contrast between these two scenarios is stark. Digital health tools, including auto-scheduling, mobile EPR access, virtual consultations, and remote patient monitoring, significantly enhance efficiency.
According to Greenhalgh et al. (2022), telehealth reduces unnecessary in-person visits, allowing healthcare professionals to prioritise urgent cases more effectively. Remote patient monitoring, as demonstrated in a study by Kitsiou et al. (2021), improves chronic disease management, reducing hospital admissions by up to 50% for conditions such as heart failure and diabetes.
A report by the King’s Fund highlights how digital tools reduce clinician burnout, with automated scheduling and mobile record-keeping cutting down on paperwork and administrative stress. Stacey’s experience illustrates this well—by eliminating time-consuming manual tasks, digital health lets her focus on what truly matters: patient care.
Challenges and Considerations
Despite its advantages, digital health is not without challenges. Infrastructure and connectivity issues can limit access in rural areas, and some clinicians may struggle with technology adoption (Shaw et al., 2018). There are also concerns about digital exclusion—patients without internet access or digital literacy may find virtual consultations inaccessible.
Moreover, interoperability remains a key issue. Many digital health solutions still operate in silos, requiring seamless integration with existing NHS systems to unlock their full potential (Murray et al., 2022). Addressing these barriers requires ongoing investment in training, IT infrastructure, and patient education.
The Future of Community Healthcare
Stacey’s story demonstrates how digital health can change community nursing. As AI-driven scheduling, wearable technology, and remote patient monitoring continue to evolve, the role of the community nurse will become increasingly proactive rather than reactive.
The new NHS 10 year plan, that’s currently in development, is expected to emphasise the expansion of digital-first healthcare models. With further investment and policy support, the future will see community clinicians equipped with real-time data, optimised schedules, and greater flexibility in delivering care.
For healthcare providers, the message is clear: adopting digital health solutions isn’t just about efficiency—it’s about delivering better, safer, and more responsive patient care. The sooner these technologies become standard practice, the better the outcomes for both clinicians and the communities they serve.


These digital tools sound like a game changer. Would be good to see this in action.
LikeLiked by 1 person