Telehealth isn’t new, but its profile has risen dramatically since the COVID-19 pandemic. As clinics scrambled to maintain care, virtual consultations became the default for many services. But now that the dust has settled, public perception hasn’t quite caught up with reality. Misinformation and outdated assumptions continue to hold sway in public discourse, affecting patient uptake and policy support.
Let’s unpack the most common myths about telehealth—and what the evidence, including my own research in community health, actually shows.
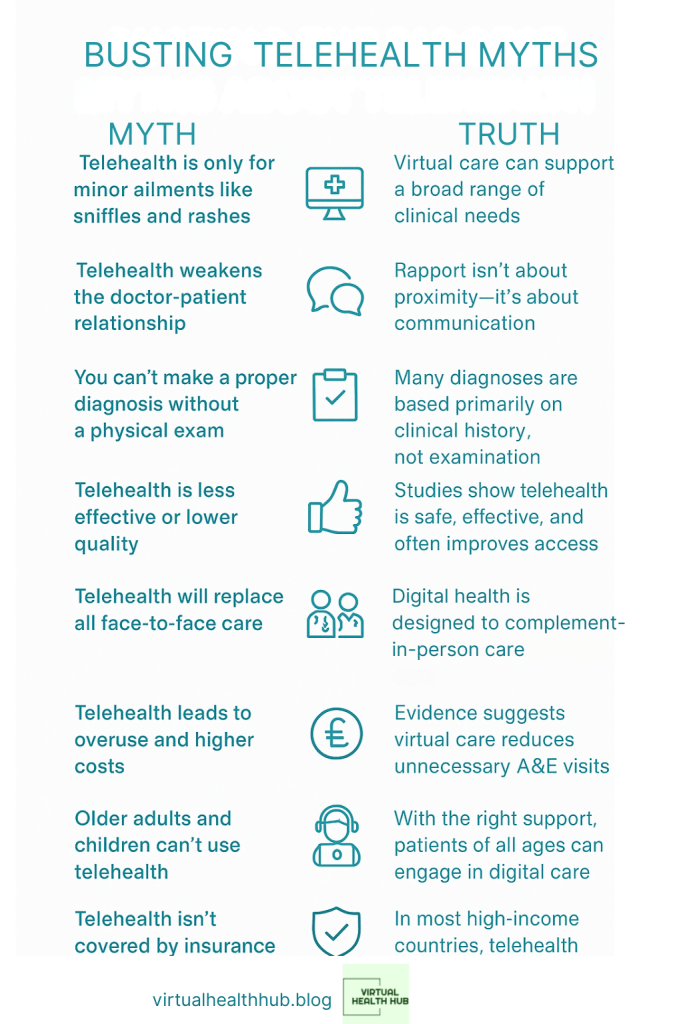
Myth: Telehealth is only for minor ailments like sniffles and rashes
Truth: Virtual care can support a broad range of clinical needs—including chronic disease management, mental health support, medication reviews, and aspects of primary care that don’t require hands-on examination.
Many conditions in primary care are diagnosed through detailed history-taking. As Dr. Laurie Jacobs from the American Geriatrics Society explains, “Listening carefully to a patient’s story often tells you 90% of what you need to know” (Equum Medical, 2024). In fact, remote consultations often improve access for those managing long-term conditions, as they allow for more regular check-ins without the hassle of travel or time off work.
Peer-reviewed research backs this up. For example, a recent review in The Lancet Digital Health found no significant difference in outcomes for virtual vs in-person care across a range of conditions, including hypertension and diabetes (Mehrotra et al., 2022).
Myth: Telehealth weakens the doctor-patient relationship
Truth: Rapport isn’t about proximity—it’s about communication.
In some cases, patients actually find it easier to open up from the comfort of home. A survey by the American Medical Association (AMA) found that 72% of patients who used telehealth reported high satisfaction with their interaction, citing convenience and a more relaxed environment as key factors (AMA, 2023).
My own research on community healthcare settings found that virtual consultations can encourage a stronger sense of continuity and patient autonomy—particularly where clinicians are consistent and make the effort to personalise communication.
Myth: You can’t make a proper diagnosis without a physical exam
Truth: Many diagnoses are based primarily on clinical history, not examination.
A well-structured consultation, whether in-person or virtual, hinges on asking the right questions. As one clinician told me during interviews for my research: “I often get more useful information from a 15-minute video call than from a rushed face-to-face with a packed waiting room.”
Where necessary, clinicians can request blood tests, imaging or refer patients for physical exams—just as they would during in-person appointments. The key difference is flexibility: virtual care allows you to triage efficiently, ensuring in-person slots are saved for those who genuinely need them (Evernorth, 2023).
Myth: Telehealth is less effective or lower quality
Truth: Studies consistently show telehealth can deliver care that is safe, effective, and in many cases, more accessible.
A 2021 analysis from Stanford Medicine found no evidence that virtual care reduces clinical quality. In fact, it often improves adherence to treatment and reduces no-show rates (Stanford, 2021). The same study noted that telehealth can reduce costs by enabling earlier interventions, especially for people with multiple conditions.
URMC (2023) reports similar findings: “Patients receiving telehealth care had similar or better outcomes in managing chronic conditions compared to in-person care—and at lower cost.”
Myth: Telehealth will replace all face-to-face care
Truth: Digital health is designed to complement—not replace—in-person care.
Some examinations and procedures will always require hands-on clinical input. But remote healthcare opens up capacity and convenience for both patients and providers. It’s particularly useful for follow-ups, medication reviews, mental health check-ins, and lifestyle counselling.
The aim is not to eliminate face-to-face contact, but to make healthcare more flexible and efficient. As Livi (2023) put it: “Telemedicine is an addition, not a substitute.”
Myth: Telehealth leads to overuse and higher costs
Truth: Evidence suggests the opposite. Virtual care can reduce unnecessary A&E visits and shorten hospital stays.
A study by the American Telemedicine Association (ATA) found that telehealth helped reduce length of stay in intensive care units by 30%—and improved early detection of complications (ATA, 2024). The perception that digital health leads to frivolous use doesn’t hold up when you look at the data.
From an NHS perspective, this is key. With workforce pressures and finite budgets, telehealth can act as a cost-saving measure by reducing avoidable admissions and enabling proactive management.
Myth: Telehealth is more prone to fraud and abuse
Truth: High-profile fraud cases exist, but they’re the exception—not the rule.
There were incidents of fraud during the pandemic, particularly in the US, as rules were relaxed to expand access quickly. But a 2023 audit by the US Department of Health and Human Services found that the vast majority of providers billed appropriately for telehealth services.
Virtual care isn’t inherently riskier—it just requires the same governance and quality assurance we expect of face-to-face care. In the UK, this means applying the same standards under CQC inspection, professional regulation, and digital infrastructure audits.
Myth: Older adults and children can’t use telehealth
Truth: With the right support, patients of all ages can engage in digital care.
Pediatric telehealth has become routine in many settings, especially for mental health and speech and language therapy. Meanwhile, older adults are increasingly digitally literate. According to Ofcom (2024), over 70% of people aged 65–74 in the UK now use smartphones or tablets regularly.
Clinicians can guide patients and carers through the process, and many platforms are designed for simplicity. All that’s needed is a device with a camera and an internet connection.
Myth: Telehealth isn’t covered by insurance
Truth: In most high-income countries, telehealth is now widely reimbursed.
In the UK, NHS contracts include digital first approaches for many services. In the US, Medicare and private insurers rapidly expanded telehealth coverage during the pandemic, and most have kept these in place (Priority Care Clinics, 2024).
The key challenge going forward is ensuring parity of funding and quality metrics—so that virtual care isn’t seen as “second tier.”
Myth: Telehealth is only useful in rural areas
Truth: Telehealth benefits both rural and urban populations.
Yes, it’s a lifeline for remote communities—but that’s only part of the story. Urban patients often face long commutes, mobility issues, unpredictable work patterns, or mental health challenges that make in-person visits difficult.
In my research with community clinicians, one GP said: “Some of my London patients prefer video calls because it means they can speak to me without needing a day off work or paying for childcare.”
Myth: Telehealth is too expensive for value-based care
Truth: Telehealth can improve safety, efficiency, and patient outcomes—all key pillars of value-based care.
Remote monitoring allows clinicians to catch deteriorating conditions early. Algorithms can flag issues that might go unnoticed in a 6-month review cycle. This proactive model supports better outcomes at lower cost, while helping clinicians focus their time where it’s most needed (Equum Medical, 2024).
The myths surrounding telehealth are persistent—but the evidence is clear. Virtual care is safe, effective, and here to stay. It complements traditional services, improves access, and supports better health outcomes across populations. For health leaders, policymakers and clinicians, the challenge now is not just to defend telehealth—but to build it into the future of care.


Great article! I wonder, though, whether the issue of broadband access, particularly in poorer or rural parts of the UK, is understated. It’s one thing to say it’s cost-effective, but for a portion of the population, unstable connectivity is a real barrier. How do we address that?
LikeLiked by 1 person